Health care providers and family caregivers often hear detailed and harrowing stories about the unfair, undeserved and often unimaginable traumatic experiences that their clients / loved ones have endured. As a result, they are at risk for vicarious trauma, also known as secondary traumatization, secondary stress disorder, or insidious trauma.
What is Vicarious Trauma?
Vicarious trauma occurs when an individual who was not an immediate witness to the trauma absorbs and integrates disturbing aspects of the traumatic experience into his or her own functioning. Friends, family members and spiritual leaders who are providing support to the survivor are also at risk for vicarious trauma. Some precursors to vicarious trauma that you might hear about are compassion fatigue or burnout.
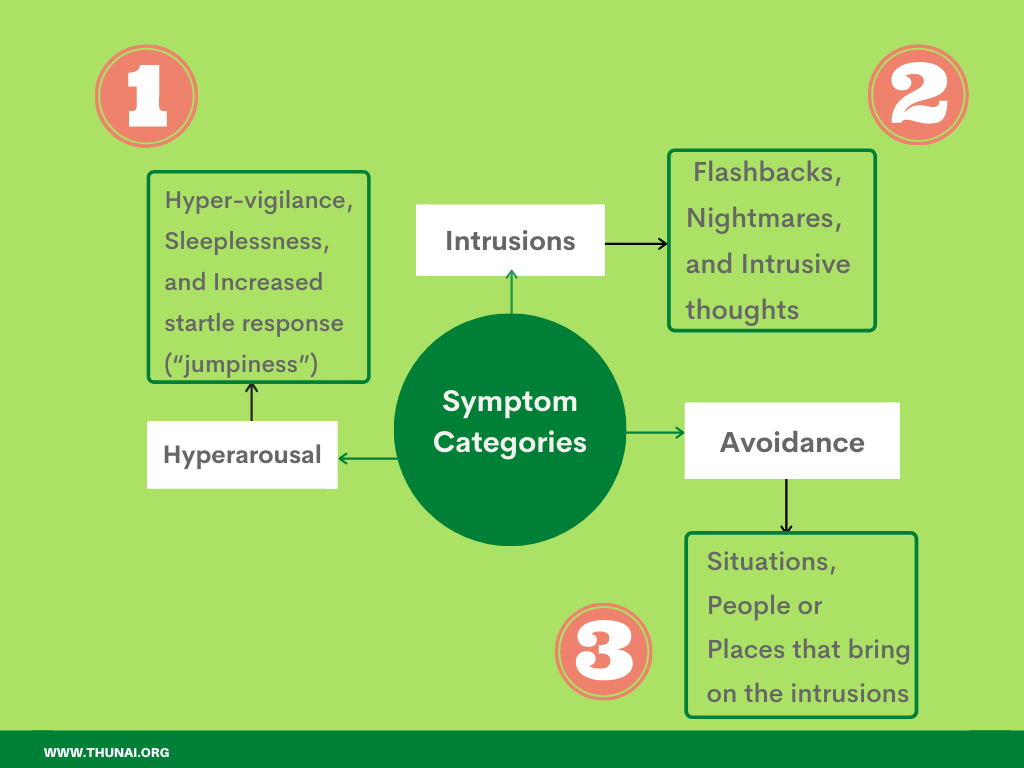
Vicarious trauma often carries many of the same symptoms as first-hand trauma or post-traumatic stress disorder. These symptoms are usually grouped into three broad categories:
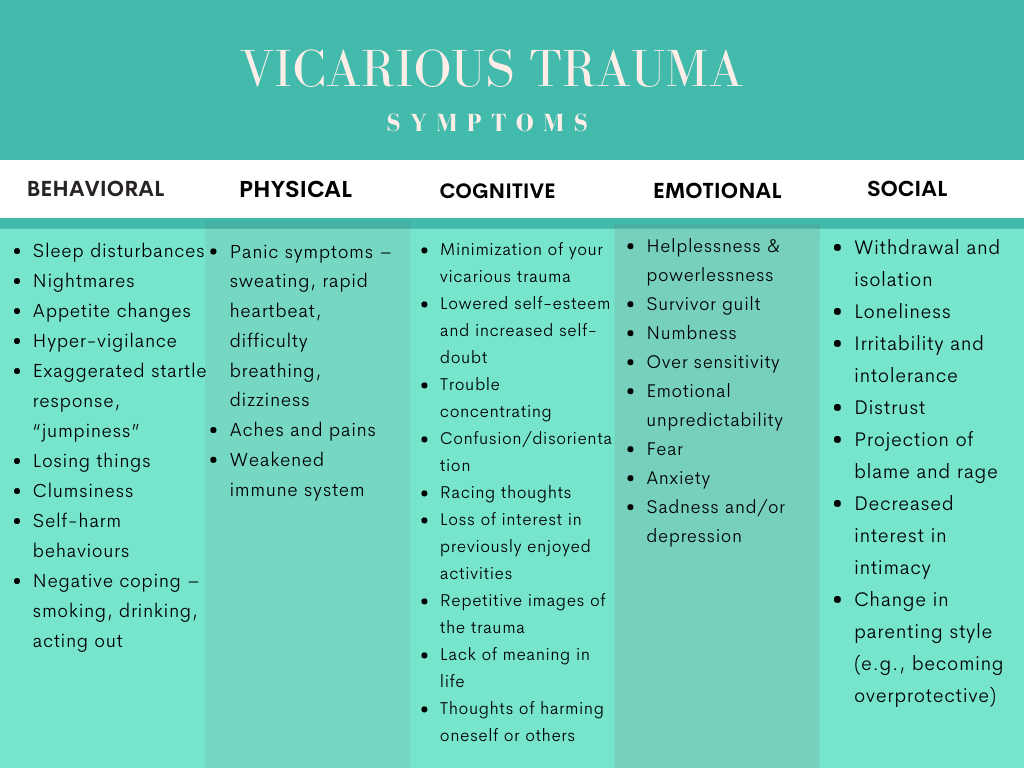
Symptoms of Vicarious Trauma
The following list provides a comprehensive picture of some of the specific symptoms you may experience.
What you can do…
Monitor yourself: In order to stave off vicarious trauma, it is important to keep track of your levels of “burnout” or “compassion fatigue”. There are several professional assessments aimed at these areas, including the Professional Quality of Life Scale, which is available online free of charge.
Take care of yourself: Just as we tell our clients, it is important for us to get enough rest, eat balanced and healthy meals and maintain a regular physical exercise routine.
Take time for yourself: Resist the urge to work without a break. Your mind and spirit need this respite. It is also critical that we take time outside of work to engage in enjoyable and restorative activities.

Separate yourself: As mental health professionals, we often provide a holding environment for our client’s pain in the counselling room. Remember to tell yourself, “This is not my pain. I am just holding it for a little while.” It is harder to do this when you see your loved one suffer but this separation is beneficial to both of you.
Limit yourself: Make sure you are maintaining proper boundaries not only with your clients, but also with your workplace. Consider limiting the number of trauma clients you see in one day, and try to vary the type of work you are doing (individual vs. group, direct vs. indirect, clinical vs. administrative). Be realistic about goals for your clients.
Help yourself: Many times, vicarious trauma takes such a toll on our lives that we need to seek professional help ourselves. Remember that you deserve this, and it will ultimately make you a better mental health care professional.
Be honest with yourself: Check in with yourself frequently to make sure you are still satisfied with your current job. Ask yourself the following questions to see what kind of mental health work you enjoy most, and to what you can to make sure you are doing what you find most rewarding.
Empower yourself: Attend professional training regularly in order to keep your skills and knowledge as sharp and fresh as possible. Develop a specialty and learn the signs of burnout within that specialty.
Renew yourself: Look for ways that you can connect with yourself on a deeper level.
Resource list
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2553228/
https://www.counseling.org/docs/trauma-disaster/fact-sheet-9---vicarious-trauma.pdf

 THUNAI
THUNAI